
Health and Care Staff Recruited to COVID-19 Vaccine Trial by NHS Greater Glasgow and Clyde and the University of Glasgow
UNITED KINGDOM / AGILITYPR.NEWS / May 22, 2020 / The University of Glasgow and NHS Greater Glasgow & Clyde (NHSGGC) are supporting the University of Oxford’s COVID-19 vaccine trials in health and care staff.
The collaboration is part of the University of Oxford’s Phase III of the trial, which involves assessing health and care staff living in Greater Glasgow and Clyde, who will be invited to take part in the trial if they are between 18-55 years old, healthy and have not been infected with COVID-19.
Frontline health, dental and care staff working in a COVID-19 clinical area such as Intensive Care Units, Emergency Departments, COVID-19 Wards, Community Assessment Centres, care homes and ambulance service are encouraged to apply. This also includes non-clinical staff such as those from portering and domestic services.
250 people will initially be recruited, with participants randomised to receive one or two doses of either the ChAdOx1 nCoV-19 vaccine or a licensed meningitis vaccine (MenACWY) that will be used as a ‘control’ for comparison.
Screening and vaccination of participants will begin in the next two weeks.
ChAdOx1 nCoV-19 is made from a virus (ChAdOx1), which is a weakened version of a common cold virus (adenovirus) that causes infections in chimpanzees, that has been genetically changed so that it is impossible for it to replicate in humans.
Participants will be involved in the trial for the next 12 months and will be supported by NHSGGC and University of Glasgow researchers throughout its duration.
The University of Oxford’s phase I trial of healthy adult volunteers began in April. More than 1,000 immunisations have been completed, and follow-up is currently ongoing.
Emma Thomson, Professor of Infectious Diseases at the MRC-University of Glasgow Centre for Virus Research and Consultant in Infectious Diseases at NHSGGC, said: “The University of Glasgow is extremely proud to be leading the phase II/III part of the University of Oxford COVID-19 vaccine trial in Glasgow in partnership with the NHS.
“An effective vaccine would be an important step forward in controlling the spread of the COVID-19 pandemic on a global scale. We will be working closely with colleagues at Oxford University to determine if the ChAdOx1 vaccine protects those who receive it from infection in a phase III clinical trial, following successful smaller phase I and II trials in Oxford.
“The vaccine will be tested initially in frontline healthcare staff in order to test the effectiveness and safety of immunisation in an at-risk group. Although we are at still at a very early stage, we remain hopeful that the information we gather will contribute to international efforts to secure a vaccine to protect those most vulnerable to infection.”
Julie Brittenden, Research and Development Director of NHS Greater Glasgow and Clyde, said: “Our staff have gone above and beyond to respond to COVID-19. We are proud to be at the forefront of research and development of COVID-19, as we take part in this vaccine trial alongside our other clinical trials. My thanks to the staff who choose to get involved in this exciting trial.”
Andrew Smith, Professor of Clinical Bacteriology at the University of Glasgow and Director of the Bacterial Respiratory Infection Service, Scottish Microbiology Reference Laboratory, NHSGGC, added: “The rapid roll-out of this clinical trial to find a vaccine for COVID-19 has been an unprecedented team effort working alongside co-workers at Glasgow Clinical Research Facility NHSGG&C, and we are super proud to be involved alongside colleagues at the University of Oxford, NHSGGC and across the UK.
“Although the point of this phase of the trial is to help us assess if healthy people can be protected from COVID-19, it will also give us valuable information on safety aspects of the vaccine and its ability to generate an immune response against the virus.”
Dr Jennifer Armstrong, Medical Director of NHS Greater Glasgow and Clyde said:
“We’re proud to have NHS Greater Glasgow and Clyde join the global effort in finding an effective vaccine for COVID-19. Our dedicated team of health and care staff have put patients first every step of the way as we responded to this virus. They now have an opportunity to get involved in research that will hopefully help patients, staff and society as a whole in future.”
Health Secretary Jeane Freeman said: “I am delighted that the Universities of Glasgow and Edinburgh along with NHS colleagues are taking part in the human safety trials for the development of a COVID-19 vaccine by Oxford University.
“Scotland has a long established reputation for medical research, and I would like to thank the research community across the country. The pace of work and the commitment of teams across Scotland has been outstanding and is testament to the world-class research infrastructure and expertise we have here.
“Of course, while the prospect of an effective vaccine developed here in the UK is exciting, there is no guarantee of success and we must continue to follow the guidelines set out by the Scottish Government to reduce the spread of COVID-19 and protect our NHS.”
The phase II/III parts of the study – involving NHS and institutions across the UK -- aims to assess how well people across a broad range of ages could be protected from COVID-19 with this new vaccine called ChAdOx1 nCoV-19. It will also provide valuable information on safety aspects of the vaccine and its ability to generate good immune responses against the virus.
The Oxford Vaccine Centre COVID-19 Phase II/III Clinical Trial Explained
What is the purpose of this research study?
The purpose of this study is to test a new vaccine against COVID-19 in healthy volunteers.
This study aims to assess how well people across a broad range of ages could be protected from COVID-19 with this new vaccine called ChAdOx1 nCoV-19. It will also provide valuable information on safety aspects of the vaccine and its ability to generate good immune responses against the virus.
What is the vaccine being tested?
ChAdOx1 nCoV-19 is made from a virus (ChAdOx1), which is a weakened version of a common cold virus (adenovirus) that causes infections in chimpanzees, that has been genetically changed so that it is impossible for it to grow in humans.
Genetic material has been added to the ChAdOx1 construct, that is used to make proteins from the COVID-19 virus (SARS-CoV-2) called Spike glycoprotein (S). This protein is usually found on the surface of SARS-CoV-2 and plays an essential role in the infection pathway of the SARS-CoV-2 virus. The SARS-CoV-2 coronavirus uses its spike protein to bind to ACE2 receptors on human cells to gain entry to the cells and cause an infection.
By vaccinating with ChAdOx1 nCoV-19, we are hoping to make the body recognise and develop an immune response to the Spike protein that will help stop the SARS-CoV-2 virus from entering human cells and therefore prevent infection.
Has the vaccine been tested on animals?
Our collaborators at Rocky Mountain Laboratories (NIAID/NIH) have conducted a rapid yet thorough investigation and demonstrated good safety and efficacy of a single dose of ChAdOx1 nCoV-19 in the rhesus macaque model that they had previously established. We were able to review the data before vaccinations in the clinical trial were initiated. There are also animal studies underway in Australia and the UK, and the results will be published once those studies are complete.
What does the study involve?
In total this study will enrol up to 10,260 adults and children across the UK.
The phase II part of the study involves expanding the age range of people the vaccine is assessed in, to include a small number of adults and children:
- Aged 56-69
- Aged over 70
- Aged between 5-12 years
For these groups, researchers are assessing the immune response to the vaccine in people of different ages, to find out if there is variation in how well the immune system responds in older people or children.
The phase III part of the study involves assessing how the vaccine works in a large number of people over the age of 18. This group will allow assessment of how well the vaccine works to prevent people from becoming infected with COVID-19.
Adult participants in both the Phase II and Phase III groups will be randomised to receive one or two doses of either the ChAdOx1 nCoV-19 vaccine or a licensed vaccine (MenACWY) that will be used as a ‘control’ for comparison.
What is the MenACWY vaccine?
The MenACWY vaccine is a licensed vaccine against group A, C, W and Y meningococcus which has been given routinely to teenagers in the UK since 2015 and protects against one of the most common causes of meningitis and sepsis. This vaccine is also given as a travel vaccine for high risk countries.
The MenACWY vaccine is being used as an ‘active control’ vaccine in this study, to help us understand participants’ response to ChAdOx1 nCoV-19. The reason for using this vaccine, rather than a saline control, is because we expect to see some minor side effects from the ChAdOx1 nCOV-19 vaccine such as a sore arm, headache and fever. Saline does not cause any of these side effects. If participants were to receive only this vaccine or a saline control, and went on to develop side effects, they would be aware that they had received the new vaccine. It is critical for this study that participants remain blinded to whether or not they have received the vaccine, as, if they knew, this could affect their health behaviour in the community following vaccination, and may lead to a bias in the results of the study.
Who can take part in the study?
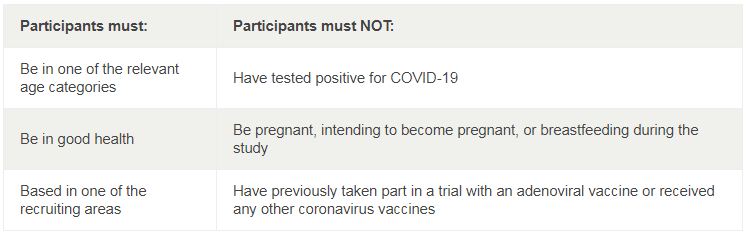
Participants must: Participants must NOT: Be in one of the relevant age categories Have tested positive for COVID-19 Be in good health Be pregnant, intending to become pregnant, or breastfeeding during the study Based in one of the recruiting areas Have previously taken part in a trial with an adenoviral vaccine or received any other coronavirus vaccines
Full inclusion and exclusion criteria is available in the participant information sheet.
How will the trial work?
The main focus of the study is to find out if this vaccine is going to work against COVID-19, if it won’t cause unacceptable side effects and if it induces good immune responses. The dose used in this trial was chosen based on previous experiences with other ChAdOx1 based vaccines.
Study participants will not know whether they have received the ChAdOx1 nCoV-19 vaccine until the end of the trial.
To recruit the large number of participants needed for this trial, multiple clinical research sites across the UK are involved in delivering the study. This is a collaborative effort led by the University of Oxford and a full list of our study sites is available on our website. Vaccinations will be taking place across the sites in May and June.
What about after the vaccination?
Some participants will be given an E-diary to record any symptoms experienced for 7 days after receiving the vaccine and if they feel unwell for the following 3 weeks. There is also a weekly survey that participants will be asked to complete about any household exposure to COVID-19.
In order to monitor exposure to COVID-19 in people who do not have symptoms, participants in some areas will be asked to collect swabs at home to be sent to the laboratory for testing.
Following vaccination, participants will attend a series of short follow-up visits. During these visits, the team will check participants’ observations, take a blood sample and review the completed E-diary and questionnaire. These blood samples will be used to assess the immune response to the vaccine.
If participants develop COVID-19 symptoms during the study, they can contact a member of the clinical team, and we will assess them to check whether they have become infected with the virus. If a participant was very unwell, we would call our colleagues in the hospital and ask them to review the volunteer if appropriate.
When will the results be available?
To assess whether the vaccine works to protect from COVID-19, the statisticians in our team will compare the number of infections in the control group with the number of infections in the vaccinated group. For this purpose, it is necessary for a small number of study participants to develop COVID-19. How quickly we reach the numbers required will depend on the levels of virus transmission in the community. If transmission remains high, we may get enough data in a couple of months to see if the vaccine works, but if transmission levels drop, this could take up to 6 months. Recruitment of those who have a higher chance of being exposed to the SARS-CoV-2 virus is being prioritised, such as frontline healthcare workers, frontline support staff and public-facing key workers, in an effort to capture the efficacy data as quickly as possible.
What if it doesn’t work?
A significant proportion of vaccines that are tested in clinical trials don’t work. If we are unable to show that the vaccine is protective against the virus, we would review progress, examine alternative approaches, such as using different numbers of doses, and would potentially stop the programme.
Contacts
Ali Howard
media@glasgow.ac.ukUniversity of Glasgow Communications and Public Affairs Office
Phone: +44 0141 330 6557 Mobile: +44 07972 280 009